Has anyone told you that therapy is a good thing?
Do you know that all therapists are not created equal?
Is it common amongst your friends and family to share mental health struggles with the same ease we do physical challenges?
Have you been shown how to access mental health services?
Do you know that you don’t have to reach a threshold in order to deserve or need therapy?
Are you aware that it’s ok to not be ok?
There are helpful tips to navigate and find an appropriate match. Read on to learn my take on mental health, therapy, and prioritizing mental wellness.

My introduction to therapy
More than a decade ago, I worked for FEMA. I joined the agency nine months before Hurricane Sandy came barreling down the east coast of the United States on October 29, 2012. In a weird confluence of events, I wound up leading the agency’s social media response to the pending hurricane and in the immediate aftermath. I was working remote in Chicago at first, then deployed in the “war room” at headquarters in Washington D.C., and finally on the ground at the joint field office in New York. I worked more than 12 hours a day, sometimes without breaks, for more than 35 days straight. I truly believe Hurricane Sandy caused my immune system to lose its tenuous hold and succumb to multiple sclerosis.
When I returned from New York, exhausted, depleted, and unwell, I was expected to resume my normal work immediately. Nobody, at that time (gosh I hope things have changed) helped or guided me. No one offered me a different path. I thought I was crazy for not being able to resume normal life. This wasn’t my first deployment but it was definitely the biggest to date. I couldn’t figure out the words to describe how not OK I was. I remember telling my boss — still deployed in DC at the time — that I didn’t know what to do. He informed me that I was welcome to use my PTO, but reminded me that he was still working and doing just fine. He also asked when I would be willing to re-deploy to New York or New Jersey.

Back then, I took that leadership and guidance as affirmation that something was wrong with me. Everyone else could cope, why couldn’t I? I would love to go back in time and say a few different things to that particular manager. One of my colleagues and dear friends, who I saw last year in Mexico, had extensive experience in disaster response and was the first person to acknowledge that my feelings were normal. I still hear their voice saying “all feelings are ok” over and over to me. They validated my feelings and halted the comparative voice ruling my thoughts and gaslighting my own feelings. saying I should be ok, should be better, should just move on.
That friend was comfortable with a whole different vocabulary — one of self care, therapy, mental health and mental struggles, and they were open about discussing these complex issues. They asked if I had ever seen a therapist. I told them no. I believe I said some asinine and ridiculous statement that I didn’t deserve therapy or help. I believed, at that time, that I had a great life, secure, safe, privileged, stable, supportive parents, family, and friends. It didn’t matter what I had just gone through, I should be ok.
At their urging, I called my insurance, found a provider accepting new patients, and within walking distance of my office, and made my first appointment. I went, we talked, I hated every minute. The woman had a yellow legal pad, wrote a few notes, and nodded the entire time. THE WHOLE TIME. I still think of that woman as a bobble head. But going into the first session with no source for comparison, I had no idea what to expect.
I returned from therapy, informed my friend loudly and with conviction, that therapy wasn’t for me and never went back to that provider.
A new diagnosis
Less than seven months later, I was diagnosed with MS. Dumbfounded, in utter disbelief, numb, and also raging, I had no way to process my inner turmoil. I was unprepared and ill-equipped to deal with the magnitude of this life change. My same friend (they really are the best, I love you Jen), told me that you need to try on therapists like you try on clothes. Not everyone is a perfect fit. Keep looking, keep trying. They informed me that there were therapists who specialized in different life events. Mind blown. I truly thought a therapist was a therapist, it never occurred to me that they specialized. I did a search for therapists who specialized in new diagnosis, who treat women, and was a woman.
I found a therapist I knew instantaneously was my perfect match. A unicorn who showed me how therapy is supposed to feel and what it’s like when it clicks. I saw her every other week to start and eventually every month consistently, until I moved out-of-state. Mind blown. Life altered. Feelings on therapy irrevocably changed.
My sister recently gave the analogy of hair cuts and therapists. How many people have cut your hair in your lifetime? If you received a bad haircut, would you never get another haircut again? No. You try another. You go back. You keep looking.
Mental health in the conversation
I began chatting with my friends about therapy — openly and without concern. My beloved Chicks & Chow dinner group would discuss the differences in our therapists, what we learned, how we were coping, and what things we were working on. Mental health — or our struggles — was not taboo. There was no stigma; no need to project an “ok-ness.” Our struggles and triumphs were as much a part of our discussions as bad dates and relationships. In hindsight, I know I was not as open with my family members as I was with my close friend group. I wasn’t ashamed, but I also wasn’t advocating for mental health access or touting why I needed it and if or how it was helping.
More than a decade ago it was a different time in the mental health landscape. I don’t remember corporate initiatives to meditate your burnout away with apps, or free counseling and therapy sessions as part of your benefits package. If any of my immediate family members were seeing therapists, I did not know. The conversation is still emerging from the shadows of stigma to stand alongside the needs of our physical health and wellbeing.
My dream team
After years of trial and error, I now have three individuals dedicated to different aspects of my mental health. In comparison to my other medical teams, three seems like a small number dedicated to my care. However I know, most people don’t have three therapists. So once again, let me reiterate and say it loudly for those in the back row, MENTAL HEALTH DESERVES YOUR ATTENTION TOO! If you believe in the mind/body connection, you have to nurture both for integrated health. Take what you need, ask questions, ask for guidance. There is help out there. Plus in this post-COVID world, so many sessions are now done from the comfort of your own home in a virtual visit. It’s never been easier to get connected to the assistance needed and deserved.
Therapist #1: Work complaints go here
As part of my benefits package we have a program that offers six free counseling sessions a year that are kept out of your medical record. A friend and colleague gave me a specific name of a woman and after one session, she’s been by my side for almost five years. I only get six sessions a year, but I space them out and use each and every one, each and every year. She provides an outlet to vent about work and it feels not only safe but intimate, because she also works there so she knows the organizational culture and dynamics. I can conserve my energy and optimize our time because I don’t have to explain. We have a shared language and foundation to jump off from and hit the ground running — metaphorically speaking that is.
When approached by a coworker with their own struggles or asked outright for a recommendation, I pass on her name without reservation.
Therapist #2: Disease-specific therapy
Last year, in the hospital with shingles, during rounding by the entire neurological team, a young soft-spoken woman introduced herself as one of the newer MS-specific therapists. She offered to begin seeing me immediately if I was interested. At rock bottom, I needed help. I didn’t know what I needed or how to feel better, but I needed a partner who could help me make sense of my inner struggles, pervasive anxiety, and debilitating depression.
She is great, and I’ve seen her monthly ever since that day in the hospital. Not only does she understand MS, but she is part of my coordinated, multi-disciplinary care team. Always with my permission, she can coordinate directly with my neurologist and share feedback, pain points, medication discussion and coordination, and frustrations in the hopes of not only improving my patient care, but improving the care coordination for others who have MS.
Therapist #3: Trauma-informed therapy
Much like my use of the F-word, FALL, I used to be (and maybe still am) scared of the T-word. I used to feel that I was undeserving of Trauma with a capitol T or even trauma with a lowercase t, as if someone, somewhere had it mapped out. I pictured a hierarchy of trauma and I didn’t meet the minimum requirements. In a fairly recent session, my MS therapist said, “I think you need trauma-specific help.” But she didn’t just drop that truth bomb and end our session. She said, “Are you familiar with PsychologyToday.com?” Fairly well-versed in navigating the complexities of healthcare in the U.S., no I wasn’t familiar.
In fact, I had never heard of this resource.

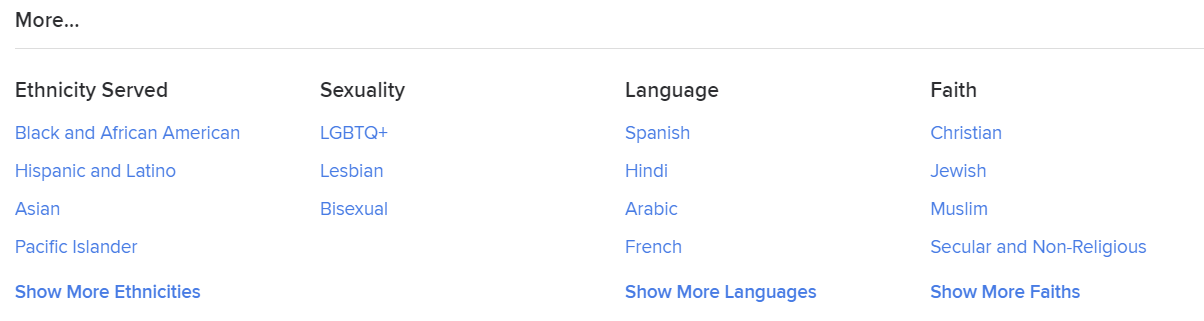
During our virtual session, she screen shared and showed me the website. She input my zip code, my insurance, and showed the myriad of options I could select when choosing a provider. I had no idea. I could choose sexuality, language, or faith. But there was also a mega menu of options of things I had never heard of that could help connect my exact needs to trained and specialized therapists. People who practiced EMDR or specialized in trauma.
It wasn’t just that she said what she thought I needed; she knew that particular help wasn’t her. She admitted her limitations and guided me to additional help. She literally showed me the way.

Big T or little t – it doesn’t really matter
Regardless of the trauma-specific label, my trauma (or Trauma) was validated. I was connected with a therapist I instantly meshed with. I feel lucky stating that I think, two sessions in, I’ve found my second unicorn. I gave my therapy elevator speech of the list of intense life experiences and challenges I’m facing as a jumping off point for working together. The provider said, “Yes, that’s trauma and you’re having a natural trauma-response.”
Having difficult feelings validated is priceless. Being seen and heard is invaluable. A big part of my healing has been telling my story. But I also need feedback, guidance, and tools to continue. The work is hard. The self reflection is constant. Some of the observations she made during our sessions knocked the air from my lungs. It’s not combative or adversarial, but it is hard to see, hear, and feel. There’s a lot to process when a concerned stranger shines a light and provides clarity on the darkest parts of your life that have made you feel lost, confused, and less than for so long. It requires honesty and vulnerability and the want to share my story and the investment in getting help. The phrase so often used is “willingness to put in the work.” It was important for me to believe relief was possible.
I’m in a place where I am consciously and actively prioritizing my mental health. While not previously neglected, it hasn’t been center stage in the last two years. My body was the acute need during transplant and immediate recovery. But processing trauma, setting clear boundaries, reframing my relationship with my health, wellness, illness, diagnosis, and body is crucial to continued healing and the possibility of moving through the trauma and pain, forward. After 11 years, perhaps I can move past anger and denial and through the other stages of grief.
I want to work to invest in a future that I have all but dismissed during the last two years in the midst of disability. I wouldn’t know I needed that without my mental health team guiding me along the way.
I hope you didn’t need this reminder to inherently trust and know that it is ok to not be ok. There is help. And, I hope you already knew how to access care in the U.S. with a well-designed website.
But if you didn’t know about that resource, or no one has ever shown you a different conversation about mental health, I am here.

